This article is a simple refresher to pelvic anatomy, what we mean by ‘stability’ and how we can optimise this in wheelchair sitting. Clinical evidence to support this blog is listed at the end.
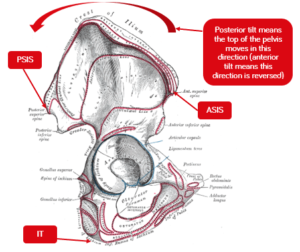
There are key pelvic landmarks we refer to during assessments for wheelchair seating.
- Anterior superior iliac spine (ASIS) which are the top front points of the hip bones when resting your hands on your hips,
- Posterior superior iliac spine (PSIS) often marked by dimples or indents on our lower back where the PSIS are close to the skin, and
- Ischial tuberosities (ITs) which are the sharp points you feel when sitting on a hard surface
 |
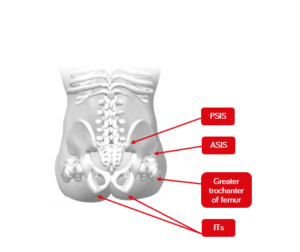 |
| Figure 1. Lateral view of the pelvis | Figure 2. Posterior view of pelvis in sitting |
We are concerned with whether these landmarks are in an anatomically ‘neutral’ position meaning that the pelvis isn’t twisted with one side more forward than the other (pelvic rotation), lower on one side (pelvic obliquity) or angled forward/backward when looking at the side-view of the pelvis (anterior/posterior pelvic tilt) and creating secondary complications to the spinal alignment. A neutral sitting position also refers to the correct alignment of the spine, head, and neck in relation to the spine and where the line of gravity falls over the pelvis (Neville, 2005).
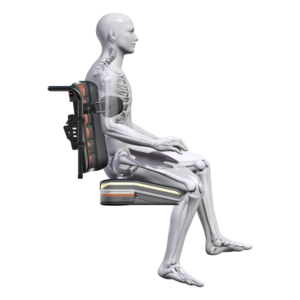
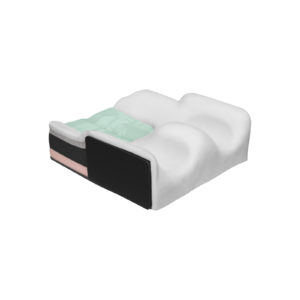
The anatomical shape of the ITs is curved (see Figure 2 above), and this can create pelvic instability as there is no flat surface on which to balance. Also the pelvis tends to tilt a little backwards in sitting and, although this may provide for added stability when reaching (Sprigle et al., 2003) the normal curves of the spine need to be maintained – if the pelvis is too forward on the seat in relation to the back rest (contributing to posterior pelvic tilt) or if it tilts too far backwards (increasing posterior tilt) this can increase the risk of developing decubitus pressure ulcers (Kobara et al., 2008) and result in hyper kyphosis and loss of the lumbar curve (see Figure 3). We need to optimise the tilt of the pelvis to alleviate the risk of pressure area development and secondary spinal deformities, and we need to control rotation and obliquity for a good sitting posture (Samuelsson et al., 2009).
backwards in sitting and, although this may provide for added stability when reaching (Sprigle et al., 2003) the normal curves of the spine need to be maintained – if the pelvis is too forward on the seat in relation to the back rest (contributing to posterior pelvic tilt) or if it tilts too far backwards (increasing posterior tilt) this can increase the risk of developing decubitus pressure ulcers (Kobara et al., 2008) and result in hyper kyphosis and loss of the lumbar curve (see Figure 3). We need to optimise the tilt of the pelvis to alleviate the risk of pressure area development and secondary spinal deformities, and we need to control rotation and obliquity for a good sitting posture (Samuelsson et al., 2009).
Figure 3. Example of posterior tilt of the pelvis and contribution to hyper-kyphosis
Essentially what we aim for is:
- ITs to be level on the seat
- Pressure loading to be shared across ITs, greater trochanters, and posterior superior iliac spines
- Pressure loading also be taken through the back of the thighs (in a manner that doesn’t pull the pelvis forward or cause the pelvis to tilt backwards/forward), arms, back, feet and head (if required) to optimise comfort
- Pelvic rotation, posterior tilt, and obliquity to be controlled or minimised to prevent secondary postural asymmetry, and
- Provide a stable seated foundation that the spine, shoulders, head, and neck can be aligned above the pelvis with the line of gravity falling through the centre of the pelvis and the anatomically neutral curves of the spine maintained.
The human body is inherently unstable – our body parts move independently to one another and our central anchors of pelvis and spine and shoulders can move in multiple directions in relation to each other. If the body’s neurological system is affected (sensory loss, muscle tone changes, muscle weakness, impaired coordination) and muscles can no longer support a neutral alignment, then these joints become even more unstable and this affects the functional ability to use our arms and legs and head freely. The human body is amazing and complex.
Stability refers to the energy or effort required to create imbalance, where our line of gravity falls outside of our base of support. Person A (below) is stable, person B is less stable as the line of gravity is now at the front of his base of support. To make himself more stable, person C simply needs to step forward and lower the load, so that the line of gravity again falls within the centre of the base of support.
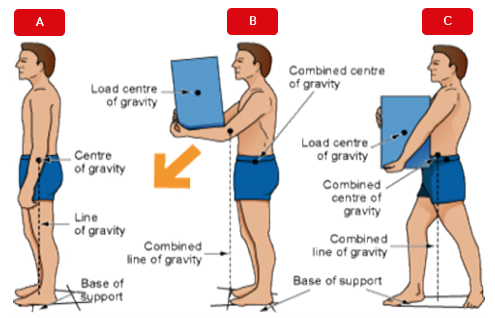
This Photo by Unknown Author is licensed under CC BY
Our base of support in standing is created by our feet, which have the only contact with the supporting surface. Of course, high heels reduce the contact we have with the supporting surface, move our line of gravity forward in relation to our base of support and raise our centre of gravity, making us less stable – less energy would be required to knock one over compared to if one was wearing flat shoes.
Sitting can be less stable than standing because of the curved shape of the ITs now bearing most of the upper body weight, and the potential for rotation, obliquity and tilt based on our sitting posture on the seating surfaces. Instability can also be inherent because of changes to one’s musculoskeletal and neurological systems affecting the positioning of the pelvic, which is the “keystone” (Pope, 2007) of posture.
Now let us consider the pelvis anatomical position and its effect on stability:
- Pelvic obliquity – one side is lower than the other meaning that most of the body weight is on one IT and the upper body must balance on a smaller bony surface. This creates a knock-on effect on the spine and the hip joints which will adjust their position to regain that stability and, potentially, to offload increased pressure. This can effectively contribute to twisting in the spine and trunk (scoliosis), changes in hip joint position (hip flexion asymmetry) and require more effort and energy to maintain sitting posture.
- Pelvic rotation – if the pelvis is level but rotated, weight is still transferred across both ITs, but rotation can cause the spine to twist which makes sitting more effortful.
- Pelvic tilt – tilt either forwards or backwards requires the muscles to hold the position and again make sitting more effortful. This affects the curves of the spines. Pelvic position, which affects posture of the upper body, can affect vital functions, like breathing, and movement of the upper extremities.
Failing to create pelvic stability (by reducing/stabilising presenting postural asymmetry) means pressure distribution can contribute to skin integrity risks, sitting becomes effortful, function of the arms and head potentially more difficult and secondary complications of postural alignment can develop or become exacerbated. The pelvis position can affect vital functions such as breathing (Lin et al., 2006), reaching ability (Samuelsson et al., 2003; Myhre & von Wendt, 1991) and therefore stability and function in sitting need to be simultaneously considered.
- Ágústsson, A., Sveinsson, Þ., & Rodby-Bousquet, E. (2017). The effect of asymmetrical limited hip flexion on seating posture, scoliosis and windswept hip distortion. Research in Developmental Disabilities, 71, 18–23. https://doi.org/10.1016/j.ridd.2017.09.019
- Amos L, Brimner A, Dierckman H, Easton H, Grimes H, Kain J, Bednarski J, & Moyers PA. (2001). Effects of positioning on functional reach. Physical & Occupational Therapy in Geriatrics, 20(1), 59–72.
- Babinec, M., Cole, E., Crane, B., Dahling, S., Freney, D., Jungbluth-Jermyn, B., Lange, M. L., Pau-Lee, Y.-Y., Olson, D. N., Pedersen, J., Potter, C., Savage, D., & Shea, M. (2015). The Rehabilitation Engineering and Assistive Technology Society of North America (RESNA) Position on the Application of Wheelchairs, Seating Systems, and Secondary Supports for Positioning Versus Restraint. Assistive Technology, 27(4), 263–271. https://doi.org/10.1080/10400435.2015.1113802
- Kobara, K., Eguchi, A., Watanabe, S., & Shinkoda, K. (2008). The influence of the distance between the backrest of a chair and the position of the pelvis on the maximum pressure on the ischium and estimated shear force. Disability and Rehabilitation. Assistive Technology, 3(5), 285–291. https://doi.org/10.1080/17483100802145332
- Lange, M., & Minkel, J. (2018). Seating and Wheeled Mobility: A Clinical Resource Guide. Slack Incorporated.
- Myhr, U., & von Wendt, L. (1991). Improvement of functional sitting position for children with cerebral palsy. Developmental Medicine and Child Neurology, 33(3), 246–256. https://doi.org/10.1111/j.1469-8749.1991.tb05114.x
- Neville, L. (2005). The Fundamental Principles of Seating and Positioning in Children and Young People with Physical Disabilities. University of Ulster.
- O’Sullivan, S. B., Schmitz, T. J., & Fulk, G. (2019). Physical Rehabilitation (7th ed.). F.A. Davis.
- Pope, P. (2007). Severe and Complex Neurological Disability. Elsevier. https://doi.org/10.1016/B978-0-7506-8825-3.X5001-5
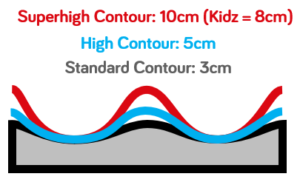
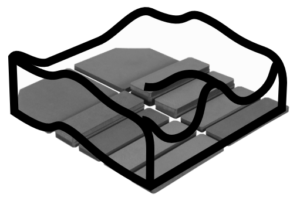
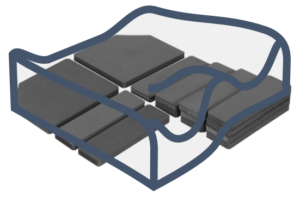
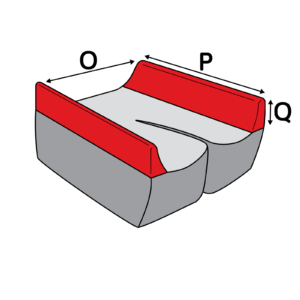
- Samuelsson, K., Bjӧrk, M., Erdugan, A.-M., Hansson, A.-K., & Rustner, B. (2009). The effect of shaped wheelchair cushion and lumbar supports on under-seat pressure, comfort, and pelvic rotation. Disability & Rehabilitation: Assistive Technology, 4(5), 329–336.
- Sprigle, S., Wootten, M., Sawacha, Z., Thielman, G., & Theilman, G. (2003). Relationships among cushion type, backrest height, seated posture, and reach of wheelchair users with spinal cord injury. The Journal of Spinal Cord Medicine, 26(3), 236–243. https://doi.org/10.1080/10790268.2003.11753690